Understanding and practising preventative health care
While seeking care when ill is important, preventative measures can help avoid many health issues entirely. Preventative care includes regular check-ups, healthy habits like diet and exercise, and timely screenings to maintain and improve your health.
The following information is based on guidance from experts in preventative medicine.
The basics of healthy living
While age and genetics are beyond your control, you can positively influence many aspects of your health through diet, lifestyle choices, and managing environmental factors, improving your overall wellbeing.
Eat a healthy diet. Prioritising a healthy diet is one of the most important things you can do for your health. Eating well can help to prevent or manage several chronic health conditions such as heart disease, high blood pressure, type 2 diabetes, fatty liver, obesity and stroke. A balanced diet provides essential nutrients like vitamins and minerals that your body needs to stay healthy and fight disease.
For most people a healthy diet includes a variety of foods with a focus on plant-based foods. Your diet should include fibre-rich food like root vegetables, whole grains, or legumes, and protein-rich options such as fish, lean meats, soya products, and low-fat dairy. Healthy fats should come from sources like nuts, seeds, fish, avocados, and other plant-based oils. Limit highly processed foods, salt, added sugars, saturated and trans fats when possible. If you have a chronic health condition, work with a dietitian to find an appropriate dietary plan that will benefit your health.
Some nutrients can be difficult to get from food alone. In many places in the world people do not get enough Vitamin D from food or sunlight at certain times of the year. Ask your GP or a dietitian if you need to take a supplement. Women who could become pregnant should take a daily multivitamin containing folic acid to prevent certain birth defects.
Stay physically active. Regular exercise is vital if you are to maintain good health. Physical activity can help prevent heart disease, obesity, high blood pressure, diabetes, arthritis, and osteoporosis. It can reduce the chances of mental health problems such as anxiety and depression and improves psychological wellbeing. It also enables you to maintain a healthy weight, reduce stress, improve sleep, and enhance overall wellbeing. So aim to get 20 to 30 minutes of aerobic exercise on most days of the week through activities such as brisk walking, jogging, swimming, cycling, tennis, or any other physical activity you enjoy. Ideally, you should also incorporate strength training at least twice a week to build muscle and maintain bone health. Incorporating stretching and mobility exercises to improve flexibility will help reduce muscle tension, enhance recovery and decrease your risk of injury. Short bursts of activity, such as three 10-minute sessions, can be just as effective as one 30-minute session.
It is never too late to start an active lifestyle. No matter how old you are or how unfit you feel, research shows that starting a more active lifestyle can make you healthier and improve your quality of life. Knowing where to start can be overwhelming, however focusing on consistency and making exercise a regular part of your routine is the most important goal. Starting with an exercise you enjoy will help with motivation to continue. If you don’t know where to start, it can be as simple as a 10min walk that over time progresses into a more well-rounded routine. If you have a medical condition, discuss with your GP the type and level of exercise that’s appropriate for you.
Aim for good quality sleep. Sleep is crucial for overall health, affecting everything from hormone regulation, weight management, heart disease to accident risk. Aim for 7-9 hours nightly with consistent sleep-wake times. To improve sleep:
- Create a sleep-friendly environment: cool, dark, and quiet.
- Keep electronics out of the bedroom.
- Use 'do not disturb' mode or a standalone alarm clock to minimise distractions.
- Limit evening screen time, caffeine, large meals, and intense exercise.
- Establish a relaxing bedtime routine.
Drink alcohol in moderation. Alcohol consumption increases the risk of liver disease, heart problems, certain cancers, accidents, and mental health issues. It can also negatively affect relationships and work performance. The World Health Organization (WHO) states there are no health benefits to alcohol consumption and that 'less is better' for overall health, regardless of specific national guidelines.
Stop smoking. Don’t smoke or use other tobacco products. Quitting smoking improves lung function, reduces risks of heart disease and cancer, increases energy, saves money, protects others from second hand smoke, and improves overall health. These health benefits begin immediately after stopping and continue to accrue over time, regardless of your age or how long you've smoked. Your GP can help develop a strategy to stop smoking using medication, nicotine replacement therapy, or behavioural support techniques.
Avoid recreational substance use. Recreational drugs and misuse of prescription medicines, including opioids, can lead to serious physical and mental health problems. These risks include addiction, organ damage, and increased susceptibility to infectious diseases such as HIV, Hepatitis B and Hepatitis C. If you're struggling with substance use, your GP can recommend confidential help and treatment options. Cannabis remains a subject of debate among experts, particularly regarding occasional adult use. However, two key points are widely accepted: firstly, heavy and prolonged cannabis use can lead to significant physical and mental health risks, including cognitive impairment, cardiovascular issues, and potential dependency; secondly, cannabis use by children and adolescents is especially harmful due to its negative impact on brain development. While research continues, these core findings guide public health approaches to cannabis use and regulation.
Follow safety procedures. Adhering to basic safety guidelines can prevent numerous serious injuries. At home, install smoke detectors, ensure adequate lighting in hallways and stairs, and eliminate tripping hazards. When out, always wear seat belts while driving, never operate vehicles under the influence of alcohol or cannabis, use appropriate safety helmets for activities like motorcycling, skateboarding, or cycling, and strictly follow workplace safety protocols.
Take the right medications and doses. Before consuming any medicine, ensure that you fully understand its purpose and proper usage. Taking too little of a medicine can prolong symptoms, while taking too much increases the risk of side effects. Follow the instructions of your pharmacist or GP. Never use medicine that has been prescribed for someone else, even if your symptoms appear to be identical. Follow your GP’s advice on completing antibiotics to prevent resistance.
Limit sun exposure. Excessive ultraviolet radiation can lead to sunburn and skin cancers. Reduce your risk by limiting sun time, especially between 10am and 4pm, wearing protective clothing including wide-brimmed hats and sunglasses, and using broad-spectrum sunscreen that protects against both UVA and UVB rays. Sunglasses also help prevent macular degeneration and cataracts. Remember that sunscreen doesn't grant unlimited sun time.
Stay protected through vaccination. Keep your immunisations current, including annual flu injections and recommended COVID-19 boosters. Tetanus protection requires a booster every 10 years, or sooner in case of a deep or contaminated wound. If you were born after 1970 and are unsure about your MMR (measles, mumps, rubella) status, consult your GP about getting a booster dose, even if you received childhood immunisations. International travel may require additional vaccines like yellow fever or typhoid. Consult a travel health clinic or your GP well before departure.
Choose a GP before you get ill. Having a GP ensures personalised care based on your complete health history and leads to better preventative medicine outcomes. Research shows patients who regularly see the same GP receive better preventative care.
Prioritise preventive health screening
Screening tests can detect diseases early when treatment is often more effective. Your GP can advise on appropriate tests based on your age, sex, health history, and risk factors.
General health screening guidelines include:
Blood Pressure. High blood pressure can lead to heart disease, stroke, and kidney disease. Some countries recommend obtaining an updated blood pressure reading at every clinic visit, others recommend checking it at least every 1-2 years. If you have certain risk factors you may need more frequent blood pressure measurements.
Cholesterol. Elevated cholesterol levels can lead to arterial plaque buildup, increasing the risk of cardiovascular disease. Initial cholesterol screening typically begins between ages 40-50. If results are normal, rescreening is generally recommended every five years. However, individuals with risk factors may require earlier and more frequent screening. Always consult your GP for a personalised screening schedule based on your individual risk assessment, as factors like family history, lifestyle, and overall health can influence the appropriate frequency of cholesterol checks.
Blood sugar. Diabetes, characterised by chronic high blood sugar, can lead to serious complications including vision loss, kidney failure, cardiovascular disease, and lower limb amputations if left unmanaged. Generally initial screening for average-risk adults starts between the age of 40 and 45. Earlier screening is recommended for those with risk factors such as obesity, family history of diabetes, hypertension, or certain ethnicities. If initial results are normal, rescreening is typically recommended every three years, though high-risk individuals may need more frequent testing. Always consult your GP for a personalised screening schedule based on your individual risk assessment.
Emotional Health. Poor mental health can significantly impact physical wellbeing, potentially affecting cardiovascular health, immune function, and recovery from illness. Persistent symptoms such as sadness, hopelessness, or loss of interest in activities for two weeks or more may indicate depression or other mental health conditions. These symptoms can also signal other medical issues, like thyroid disorders. Many GPs now include mental health screenings in routine check-ups, recognising its crucial role in overall health. Conversely, good mental health practices, such as stress management, mindfulness, and maintaining social connections, can enhance overall wellbeing and disease resistance. Regular mental health check-ins are as important as physical health screenings. If you experience concerning symptoms, consult your GP promptly.
Sexually Transmitted Infections (STIs). Regular screening is essential for sexually active individuals, as many infections can be asymptomatic while causing serious health complications if untreated. Risk factors include multiple sexual partners, inconsistent condom use, having a partner with an STI, or intravenous drug use. Discuss appropriate screening frequency with your GP based on your individual risk factors.
Bone Health. Osteoporosis, characterised by low bone mass and structural deterioration of bone tissue, significantly increases fracture risk. While it affects both sexes, postmenopausal women are at higher risk due to hormonal changes. For women aged 65 and older and men aged 70 and older, bone density testing is routinely recommended. Earlier screening is advised for postmenopausal women and men over 50 with risk factors, including previous fragility fractures, family history of osteoporosis, low body weight, smoking, excessive alcohol consumption, or use of bone-depleting medications. Certain medical conditions, such as rheumatoid arthritis or chronic kidney disease, may also warrant earlier screening. The frequency of follow-up testing depends on initial results and individual risk factors. Consult your GP about the appropriate timing for bone density assessment based on your personal risk profile.
Oral Health. Regular dental check-ups (every 6-12 months) and good daily habits are essential for preventing dental disease. Practise proper oral hygiene by brushing your teeth twice daily with fluoride toothpaste, flossing daily, limiting sugary foods, and avoiding tobacco products. Early detection and treatment of dental problems can prevent more serious complications.
Eye health. Eye exams screen for vision changes and early signs of conditions like glaucoma, cataracts, and macular degeneration. Young adults should have at least one comprehensive eye exam between ages 20-29, then every 2-3 years from ages 30-39. Adults aged 40-64 should schedule examinations every two years, while those 65 and older should have annual check-ups. People with risk factors such as diabetes, high blood pressure, family history of eye diseases, or those taking medicines affecting vision require more frequent examinations as determined by their eye care professional.
Hearing. Regular hearing screenings are essential for adults as they help detect hearing loss early before it significantly affects daily life. These screenings establish a baseline for hearing health and can reveal potential underlying medical conditions. Early detection allows for timely intervention, which is crucial for maintaining cognitive function, social connections, and overall quality of life. Many sources recommend hearing screening after the age of 50, however any adult experiencing symptoms of hearing loss (difficulty understanding conversations, frequently asking others to repeat themselves, etc.) should get a hearing screening regardless of age.
Cancer. Early detection through regular screening can significantly improve treatment outcomes for many cancers. Screening recommendations vary by cancer type, age, gender, family history, and personal risk factors. While general guidelines exist, your GP can develop a personalised screening schedule based on your individual risk assessment.
- Colorectal: Colorectal cancer is one of the leading causes of cancer death. For average-risk individuals, screening should begin at age 45-50 and continue until age 75. Earlier screening may be needed for those with a history of polyps or family history of colorectal, ovarian, or uterine cancer.
- Skin: While there's no universal recommendation for routine screening of the general population, regular self-examination is essential. High-risk individuals—those with fair skin, personal or family history of skin cancer, history of excessive sun exposure, numerous moles, or weakened immune systems—should discuss more frequent examinations with their GP. When performing self-checks, use the ABCDE rule: watch for Asymmetry, Border irregularity, Colour variations, Diameter larger than 6mm, and Evolving size, shape, or colour. Report any concerning changes promptly to your GP.
- Prostate: Discuss the option of screening with your GP starting at age 50, or earlier (around 45) if you have risk factors such as African ancestry or a family history of prostate cancer. The decision to screen should be an individual one, based on your personal values, risk factors, and overall health status.
- Breast: Breast cancer is one of the most common cancers affecting women worldwide, but early detection significantly improves treatment outcomes. Starting at age 40 women should begin regular mammograms (frequency varies based on region and individual risk factors). Familiarise yourself with the normal appearance and feel of your breasts and promptly report any noticeable changes to your GP.
- Cervical: Regular screening is crucial for prevention. Frequency depends on age and previous results.
The future of preventative health
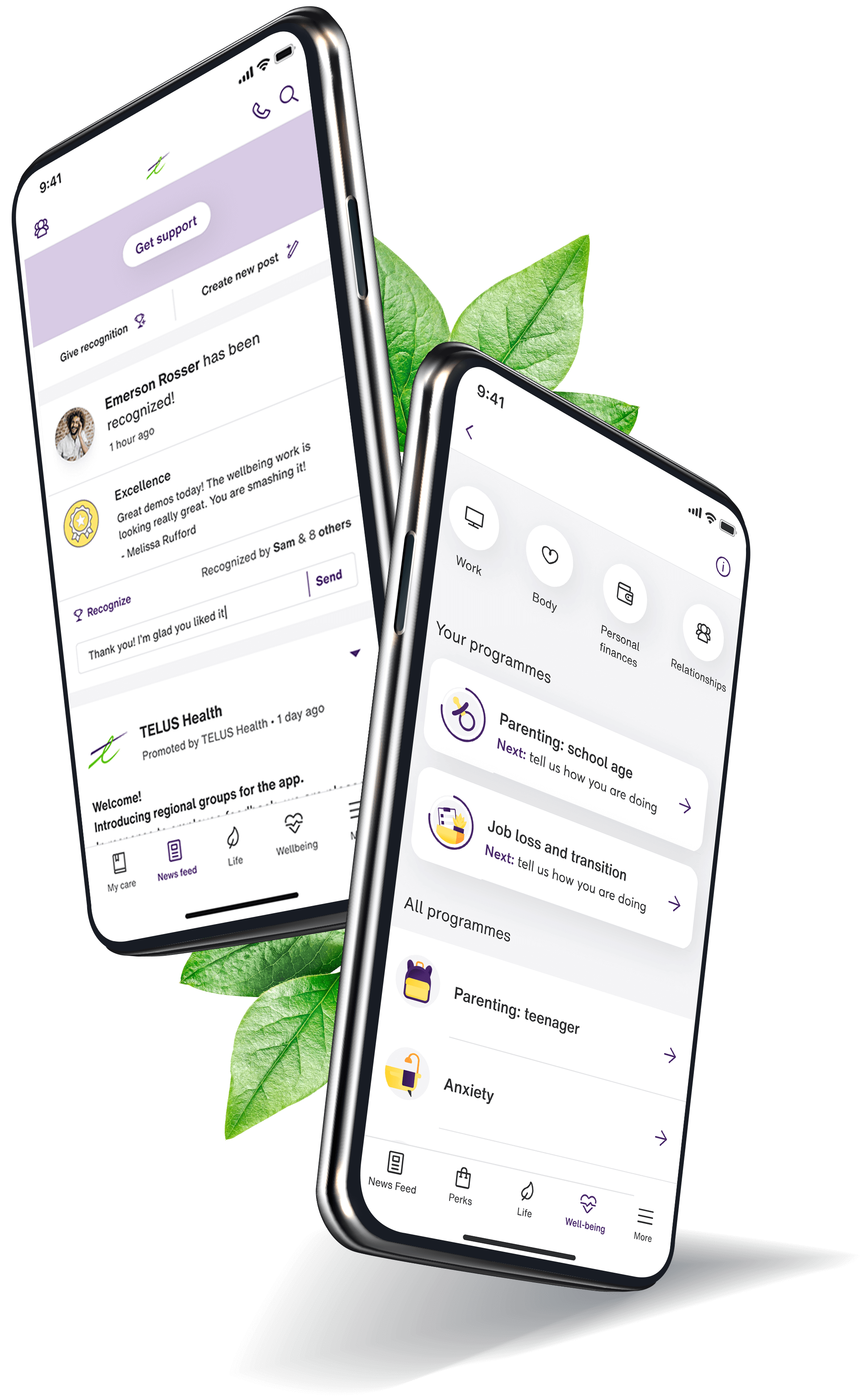
Integrated digital health tools are transforming preventative care, making health management more proactive and accessible. Wearable devices, smartphone apps, telehealth platforms, and AI-powered systems now enable:
- Real-time tracking of vital signs, physical activity, and sleep patterns such as Fitbit and Apple Watch monitor heart rate, steps, and sleep quality in real-time; or continuous glucose monitors like Dexcom which tracks blood sugar levels 24/7 for diabetes management.
- Easier access to GPs through telehealth platforms that allow patients to consult doctors via video calls; or apps that provide AI-driven symptom checks and facilitate virtual GP appointments.
- Personalised health recommendations and education with apps that offer tailored diet and fitness plans based on individual health goals; or AI-powered platforms that provide personalised insights based on symptoms and medical history.
- Medication and appointment management using apps that send reminders to patients to take medications on time; or platforms that help patients schedule, manage, and track healthcare appointments.
- Data-driven insights for both patients and GPs using platforms that aggregate data from various wearables and apps, offering actionable insights to users and healthcare providers; or Electronic Health Record (EHR) systems that provide doctors with real-time data analytics for better decision-making.
These advancements facilitate more proactive health management, allowing individuals to take greater control of their wellness journey while providing healthcare professionals with comprehensive patient data for improved care.
Making health work for you
Not everyone has equal access to health resources, but maintaining good health is still achievable within your means. Budget-friendly options include walking and home exercises, cooking with seasonal produce and legumes, accessing community resources and free health screenings, maintaining good sleep habits, and building social connections through local groups and outdoor activities. Focus on what's available to you and build sustainable habits that fit your circumstances.
Your role in preventative health care
While research in preventive medicine continues to advance, your daily choices remain crucial to your overall health. Maintaining a balanced diet, regular exercise routine, and adequate sleep, along with avoiding smoking and excessive drinking, form the cornerstones of personal health management. By following these guidelines and the preventative care recommendations outlined in this article, you significantly improve your chances of long-term wellness and reduce your risk of chronic diseases. Remember, consistent, informed decisions about your lifestyle are your most effective tools for maintaining good health.
This information is provided to supplement the care provided by your doctor and is not to be used as a substitute for professional medical advice. Always seek the advice of your doctor if you have questions about a medical condition or treatment plan.